Gene therapy is a set of techniques that involve correcting the function of a “sick” gene, often by replacing it with a functional gene (“drug gene”). A pioneer and leader in gene therapy, Genethon is working to develop gene therapies for rare diseases.
Gene therapy involves introducing genetic material into cells for the purpose of treating a patient. It is used to make the cell produce a missing or malfunctioning protein, and is thus a preferred approach for treating rare genetic diseases.
Initially developed to treat rare diseases, gene therapy is now also used or being studied for the treatment of common diseases such as cancer or degenerative diseases, and also in vaccine approaches.
Gene therapy: providing a functional version of the gene
At the heart of our cells is our genome; it is made up of around 25,000 genes, inherited from our parents. These genes are made up of DNA. If there is a defect in the DNA, or a mutation, then the gene may not function and this mutation will lead to a pathology: this is what genetic disease means. The idea of gene therapy is simple : replacing or repairing the damaged DNA.
Today most therapies approved for use in humans consist of providing a functional copy of the defective gene, using a vector that will allow the gene to penetrate inside the cells, and then express itself. The defective gene is not modified, but a healthy gene or “medicinal gene” is introduced into the cell nucleus, which will compensate for the defective function.
New gene therapy methods are now being developed, in which the aim is to correct the defective gene using “molecular scissors; this is gene editing. The best-known scissors are probably the CRISPR-Cas9: they have revolutionized this technique since they are so simple to use.
Learn more about Gene editing techniques

Gene therapy: different methods of delivering drug genes to cells
Drug genes are delivered into the cells by carriers, also known as “vectors”. These vectors are components of viruses, used for their ability to penetrate into the cell. The most commonly used viruses are AAVs (adeno-associated viruses) and lentiviral vectors.
One of the major challenges of gene therapy is to target the vectors precisely and effectively to the diseased cells and tissues.
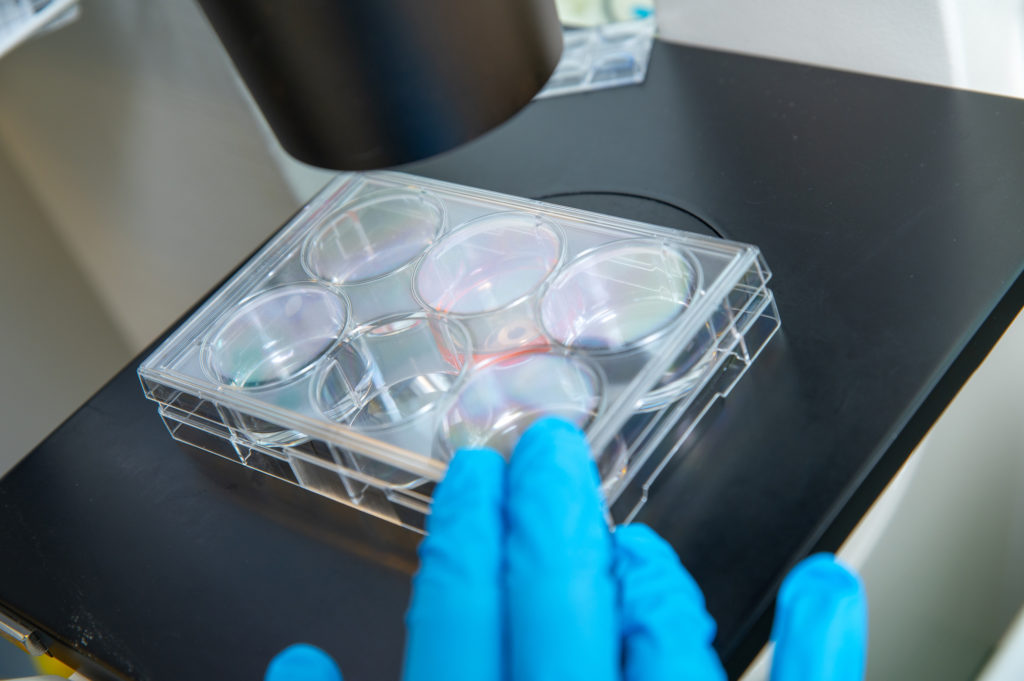
Several techniques are used. Certain pathologies, of the blood mainly, can be treated ex vivo: stem cells are taken from the blood or the bone marrow, the functional gene is added to them in the laboratory, then the corrected cells are reinjected into the body, where they will multiply. For pathologies such as myopathies, the preferred technique involves injecting the gene in vivo, or directly into the body or the organ to be treated.
Genethon is poised to face the new challenges of gene therapy
After decoding the human genome, Genethon embarked on the design of gene therapies for rare diseases in 1997. In 2006, Genethon launched the first gene therapy trial in Europe for a neuromuscular disease (gamma sarcoglycanopathy) to demonstrate the feasibility of gene transfer in humans, and in 2010, launched the first international gene therapy clinical trial for therapeutic use, for Wiskott-Aldrich syndrome, a blood disease.
Today, a first medication obtained from Genethon’s research has received marketing approval to treat spinal muscular atrophy, another is pending approval for a rare eye disease, and a third is nearing completion of its clinical trials before applying for approval.
Thirteen products from its research or to which Genethon contributed are today in clinical trial; seven others should enter clinical trials in the coming five years for rare diseases of the muscle, liver and blood.
These first victories mean that new challenges are ahead. Genethon is at the forefront in seeking to overcome the scientific and technological hurdles still linked to gene therapy. Although the vectors used have demonstrated effectiveness in a wide range of diseases, they still have limitations. For example, immune responses to these viral vectors have to be overcome in order for the therapies to be injected multiple times when the same patient needs such treatment. Some patients also have natural immunity against these vectors, which makes them ineligible for these treatments.
So we need to design more specific, more powerful and less immunogenic vectors, and develop approaches for reinjecting these treatments if necessary.
We also need to improve bioproduction methods to reduce the cost and allow large-scale production of considerable quantities of treatment for all eligible patients.
Find out more
>> Find out more about ongoing research
>> Find out more about the history of Genethon

